
17 Jun Metoprolol Tartrate – POTS Treatment (Part 1 of 3)
{This article is one of three parts in a mini-series discussing my experience with POTS treatments. Check out the second article here and the third article here.}
Oftentimes people with postural orthostatic tachycardia syndrome (POTS) are told, or assume, that there is no actual treatment for POTS. Initially, I was told that medication wasn’t an option, and to do my best with lifestyle adjustments like drinking more water, eating as much salt as I could manage, wearing waist-high compression, and doing recumbent exercise. Even just today I watched a video, and they mentioned how there is no actual treatment for POTS, only lifestyle management techniques. And while it’s not entirely incorrect, it’s also not entirely correct. Indeed, there is no FDA-approved drug to manage or ‘cure’ POTS. But that doesn’t mean there are zero treatment options. In fact, there are several drugs that are used to minimize symptoms, and while not all of them work for everyone, there is data to show that they do indeed work for some.
As a quick overview, my medical journey started with two trips to the ER, followed by an appointment with my primary care physician (PCP) who then referred me to a cardiologist. I underwent a variety of tests (EKG, Echo, Holter, Tilt Table Test, Autonomic Testing, MCOT Monitor), and the grand result was a “probable” POTS diagnosis, though I was told that there was nobody within the system who would be familiar enough with the condition to treat me. I was referred to a POTS specialist at Froedtert Hospital, but the soonest they could schedule me was in 9 months. I tried to schedule an appointment with a POTS specialist at Mayo Clinic but was informed they were not currently taking external referrals, and was overall discouraged. I was struggling to do basic tasks (like cooking/eating, showering, laundry, and errands) and had to move home to be taken care of. So hearing that I would have to wait until next year to be seen certainly kicked me into gear. After some brainstorming with family, we realized that being seen by any doctor within the Mayo Clinic system locally (not necessarily just a specialist) would be worth a shot. After all, Mayo was the first to coin the term POTS, develop the diagnostic criteria, and research outcomes. If any system would have a decent familiarity with the condition, it would be them (and I wondered if I could acquire an internal referral that might allow me to be seen in Rochester after all).
By God’s grace, I was able to go to a doctor at a Mayo System clinic in a small town in WI the following week. I knew that they may or may not be able to treat me, but it was worth a shot.
And it was.
She told me she wasn’t afraid of POTS, and that she would collaborate with her colleagues and do her best to get me on a path towards recovery. In the end, our plan included a prescription for metoprolol, a virtual follow-up check-in, and a referral to the specialists in Rochester.
{Now for a bit of speculation if you’re into POTS pathology (based on my current understanding). POTS is generally seen as one of three categories: hyperadrenergic (imbalance of the sympathetic nervous system), hypovolemic (low blood volume), or neuropathic (miscommunication between the nerves and blood vessels). With my history of PTSD and panic disorder, as well as family members having a somewhat poor adrenaline tolerance, it makes sense to me that I may lean more towards hyper-POTS. And therefore, the choice of drug (beta blocker, which shields the heart from getting jacked up on excess adrenaline) made complete sense to me. Not that I couldn’t have benefitted from boosted blood volume from fludrocortisone or the extra help with blood vessel constriction from say, midodrine, but that’s just my unfiltered and “I’m-not-a-doctor-don’t-listen-to-me” speculation.}
Week 1 of Metoprolol
Ok. Let’s get to it.
On day 1, I was scared. A little. Ok….a lot.
I’ve never really taken medications and was a little nervous about allergic reactions, side effects, or simply no improvement. My mind raced with all the questions. How does the drug actually work? Will lowered heart rate matter in the grand scheme of things? Why are nearly all my existing symptoms on the side effects list? What if my blood pressure tanks? What if my blood pressure tanks overnight and I don’t even know it?
At some point, I realized my questions had escalated from curious, to diligent, to obsessive. So I took my first dose of 12.5 mg, and immediately got to work on a computer project to keep my mind engaged. I’ll give you a quick spoiler – metoprolol has been amazing, but I’ll admit, the first day had me wondering. Within an hour I was feeling downright weird. Nothing too alarming, but I certainly was having a hard time focusing my eyes, felt pretty sleepy, and the world kinda wobbled when I walked. My blood pressure took a casual dip (from 115/67 to 95/66), and I made sure to chug water throughout the day and munched some kosher salt, as I’ve learned to do. It wasn’t until the afternoon that my BP came back over 100/60, and by the time I was due to take my second dose, I was back to a solid 123/66. I took my second dose and felt pretty chill.
And y’all. Let me tell you. While I wasn’t a fan of the lower-than-ideal dips, I was caught very much off-guard by the reality of it actually working. It did what it was claimed to do. It lowered my heart rate, first try. I stood in the kitchen to warm up some lunch, and just stood there…still. I was extremely curious what would happen. On an ordinary POTS day, if I were to stand perfectly still in the middle of my tile-floored kitchen, my pulse could pretty easily get into the 120-130s within 1-3 minutes.
But not with metoprolol! I stood there, looking at my mother, and she was looking back at me. We waited. I checked my HR. And low and behold, I was at 75bpm. I laughed. I felt SO good.
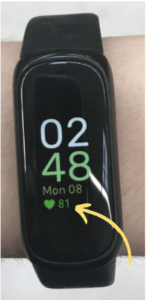
I went with her on an errand, and after scampering through the parking lot, walking through the store, and standing in one spot looking at a product, I was at a glorious 81bpm. “Mom! Look!” I said, and snapped a picture of my fitbit. I silently wondered if this delightful, grounded, steady feeling is what it’s like for normal people to feel while shopping. Was so much of my “anxiety” while out-and-about really just the tachycardia? Have my baselines really shifted THAT much?! I started to rethink the last 8 months and what symptoms actually belong to which origins.
Upon waking up on Day 2, I felt like a wet noodle, weak and utterly unable to even sit up. I wondered if my evening dose the night before was still having its effect, and sure enough, my blood pressure was 88/43. After slamming an electrolyte drink and eating some snacks in bed, I was able to sit up and had bounced back to 107/69.
On day 2 I was feeling good, and slowly started pushing the limits. Amazingly, I was met with minimal resistance. I had just moved into my new room and was putting my closet together. For months I had been wishing I had the energy to try on and purge my closet, knowing I had a year’s worth of stuff I simply didn’t need or want. But getting dressed even just once per day took significant energy, so “trying on old clothes” sounded like a nightmare. But as I watched my heart rate lower and my energy rise, I decided to try on “just one thing.” But one thing became three things, and three things became the whole box.
And that is when life as I knew it officially shifted.
I tried on shorts and a summer shirt, and for the first time in 8 months, had a flash of hope. Do you think I could wear this OUT?! Could I go visit my friend in the U.P.?! Could I volunteer at camp for a week?!
I pranced around the house and called out, “Mom!! I feel so normal!” We were both beaming.
Now wearing shorts, I was primed and ready to go outside. Neither of us knew if it was wise, but I felt so good, and with a heart rate in the 80s, I pressed on. I took our dog, Peanut, for a walk. I wanted to run and jump and the ground just felt so stable. I came back inside. Then I went to get the mail. And with every fiber of my being, I was JAZZED. I went out to the shed, gathered some seeds and a trowel, and made my way to my planter box. I sat on the porch and planted my basil. Checked in with myself, and still felt great. I planted some parsley, cilantro, chives, and radishes.
Still ok? Yes. Still ok.
By the time I got inside I was tuckered out. But for the first time in 9 months, I was ONLY “tuckered out”, not the usual “completely fatigued” or “feeling like death.”
I rested for about 20 minutes, and then my Dad came downstairs after finishing his workday. “So, are we going out for Taco Tuesday?!” he excitedly asked. Mom curiously looked over at me, and as I slowly sat up, I heartily confirmed.
After all, you don’t know the limits until you push them!
I navigated tacos LIKE A CHAMP. Stood in line, ate without getting dizzy, and arrived back home in one piece.
It felt like–and was–a miracle.
Days 3 and 4 were similar in capability, and my little mind was thoroughly boggled.
Unfortunately, I then had my first ever migraine. It was by far the most brutal “headache” I’ve ever experienced, and it wiped me out for a solid 2 days. Along with the aversion to movement, sound, and light, I felt an uptick in my normal swings in pulse and overall fatigue.
The final two days of my first week on metoprolol tartrate were alright. It was a chaotic blend of feeling AWESOME and feeling like a limp sack of potatoes. But even so, I was so grateful for this new chapter of life. The high and low swings were FAR easier to manage than straight-up POTS in the raw. I could DO things! It was a revelation.
Looking Forward
My appreciation for medicine has significantly grown over my first week on metoprolol tartrate. I have been praying for a healing miracle these past 9 months, and while it’s not a permanent solution and it’s certainly not perfect, this week I feel as though I’ve seen a glimpse of that healing. God works in so many ways, and I am so grateful to accept this help in this season.
For week 2, my doctor gave me a new prescription for metoprolol succinate, which is the extended-release version of the same drug. The goal being to lower heart rate in a slower, more steady manner. Stay tuned, for an article on week 2!
-
Making a Full Physical Recovery – A Day-by-Day Miracle
“You should exercise more.” A brutal statement. One I had tried to fulfill on my own, and time and time again, had failed. It was a frustrating piece of advice from my doctor, and felt so out of reach as I navigated my bouquet of chronic illnesses....
27 June, 2024 No comment -
Awesome Recovery News!! And Why I No Longer Plan To Write About My Symptoms
I am so excited to report that after graduating from the 3-week Pain/Symptom Rehabilitation Center at Mayo Clinic in Rochester and continuing the program at home, I am nearly 100% recovered!...
05 March, 2024 3 Comments -
What is the Valsalva Maneuver like?
The Valsalva maneuver is EASILY the most fascinating thing I’ve gotten to do in this entire medical adventure. On the surface, it’s a fairly quick and easy part of autonomic testing, but underneath, it’s one of the coolest and most complicated mechanisms of the human body that I’ve encountered. ...
17 January, 2024 3 Comments





Pingback:Week 2 of POTS Treatment - Metoprolol Succinate - Kaley Faith
Posted at 11:33h, 19 June[…] {This is the second article in a mini-series on treatment options for POTS. Check out the first article here.} […]